|
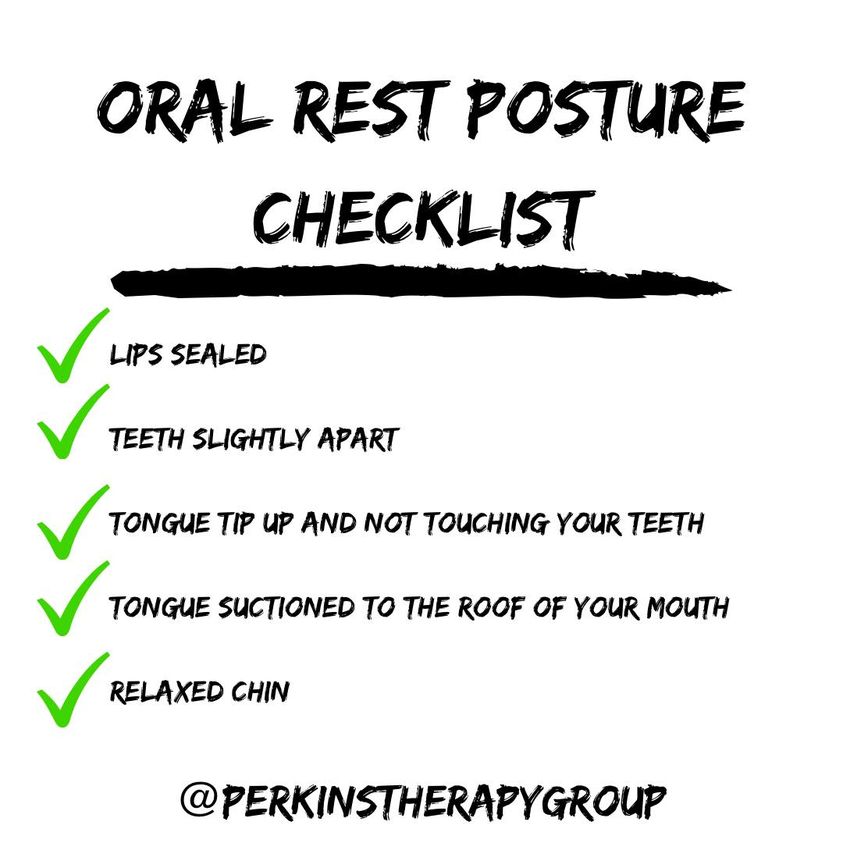
When you aren’t using your mouth your lips should be sealed, your teeth slightly apart, your tongue tip should be up and not touching your teeth, your tongue should be suctioned to the roof of your mouth and your chin should be relaxed. This is optimal oral rest posture.
Optimal oral rest posture > Suboptimal oral rest posture I encourage you to strive for correct oral rest posture. So why is the way you hold your mouth so important? If your lips are constantly parted this could result in mouth breathing. Mouth breathing can alter facial growth and development for the worse. If you aren’t using your nose to breathe, then your overall health is affected for the worse as mouth breathing does not provide the positive benefit that nasal breathing provides. If you constantly clench and grind your teeth, then this could result in your teeth to wear down and your temporomandibular joint could be negatively impacted. If your tongue is constantly pressing against your teeth, then this could result in your teeth shifting even after you have had braces, and your speech could be distorted due to incorrect oral placement of the tongue when talking. If your tongue is resting low in your mouth, then this could negatively impact facial growth and development, speech production, the way your teeth look, your temporomandibular joint and much more.
0 Comments
Are your lips sealed? Are your teeth slightly apart? Is your tongue resting right behind your upper teeth, but not touching your teeth? Is your tongue lightly suctioned to the roof of your entire mouth? Is your chin relaxed? If you answered no to any of these, then I challenge you to start studying your habits. Oral rest posture may seem like a strange thing to think of, but it’s important and essential to your overall health.
So what is your mouth really doing throughout the day when you are not using it? Are your lips remaining parted throughout the day? Are you clenching your teeth together? Is your tongue pressing against your teeth? Is your tongue resting low within your mouth? Is your chin all bunched up? If you mouth breathe, clench/grind your teeth, press your tongue against your teeth, rest your tongue low in your mouth, or if you have to bunch your chin up just to keep your mouth closed, then you present with suboptimal oral rest posture. Optimal oral rest posture consists of your lips together, your teeth slightly apart, your tongue lightly suctioned the roof of your mouth, and a relaxed chin. Suboptimal oral rest posture negatively impacts facial growth and development across the lifespan. Is your oral rest posture optimal or suboptimal? I just wanted to take a minute to introduce myself!
My name is Ashley, I have been a Speech-Language Pathologist for 5 years. I work in private practice and specialize in Orofacial Myofunctional Disorders (OMDs), feeding, and speech sound disorders. In March 2015, I had my first child, Michael. In May 2015, I graduated with a Master of Science Degree in Speech-Language Pathology from the University of Louisiana at Lafayette. In June 2015, I started working full-time in a Skilled Nursing Facility (SNF) setting. While navigating becoming a new mother, I was also navigating breastfeeding issues. We attended regular weight checks at the Pediatrician's office, and had several meetings with an IBCLC throughout our breastfeeding journey. I felt at a loss not knowing how to best help my son, which led me down the rabbit hole of oral function in infancy as it relates to breastfeeding and overall feeding development. Even though I felt like I did not know how to best help him at the time, despite my best attempts, I started researching and growing my knowledge base, and I have never stopped. In addition, while figuring out how to maintain our breastfeeding relationship, I was also working in a SNF and managing a significant dysphagia (swallowing) caseload within the geriatric population. I was simultaneously researching and learning about oral function from infancy to throughout the lifespan. I was enamored with oral function and the variability in presentation of issues seen. I had this ongoing internal dialogue and I was continuously questioning everything that I was seeing, and felt like I needed to learn even more in order to best help my son as well as all of my other patients. As I was learning, I realized that not one course could fully help me to understand how to best help everyone, so I started taking course after course, and I have come to realize that the presentation of oral function deficits is so variable that even after a lifetime of studying oral function deficits that there is always something new to be learned. As my son reached the toddler age, I realized I was now feeling defeated again while attempting to expand his food inventory (the food he likes), and I was now dealing with more questions, and a picky eater. In addition, I realized my toddler son was still drooling, had a slight open mouth resting posture, poor oral rest posture with his tongue resting low and forward within his oral cavity, poor oral awareness, lisp, speech sound production errors, and was grinding his teeth during his sleep. (I did not really understand what I was seeing, but I was taking notes of it because I am that strange person who has been taking notes on my children's development since birth). In 2017, Mila was born. Mila's history consists of breastfeeding issues, bottle feeding issues, trouble managing thin liquids during bottle feeds, a submucosal tongue tie, a tongue-tie release, trouble coordinating her breathing when drinking through a straw, visually over-responsive to presentation of new foods, immature chewing pattern, poor oral awareness, swallowing food whole, tented upper lip, open mouth resting posture, forward lingual resting posture, immature swallowing pattern. Despite everything I learned within the feeding world, I still felt like I was missing something, and in 2018, I stumbled upon the world of Orofacial Myofunctional Disorders (OMDs). OMD refers to abnormal resting labial-lingual posture of the orofacial musculature, atypical chewing and swallowing patterns, dental malocclusions, blocked nasal airways, and speech problems (Hanson, 1982). This is when I realized, I was deep in a rabbit hole, and really felt like I knew absolutely nothing. Everything that I was seeing finally came full circle and had a name for it, but where would I start? How would I even begin to help my family when so many issues are present? Who would be a part of my kid's team? Orofacial Myofunctional Disorders directly impact feeding and speech, and both of my children present with Orofacial Myofunctional deficits. I needed a team who would value my insight as a mother and professional, a team who participates in regular continuing education to further their knowledge, a team who would collaborate with other members of the team, a team who would endlessly strive to research how to best help my children, and a team who would help me grow in my understanding of Orofacial Myofunctional Disorders in order to best help my family and my clients. It was no easy feat, but we have found our team. If you are questioning anything with your child or yourself, please email me at ashley@perkinstherapygroup.com. |
Ashley Perkins,
|

 RSS Feed
RSS Feed